I now have a new blog and probably will be doing most of my wrting there
It can be found Here.
Graffiti
Sunday, May 11, 2014
Tuesday, May 6, 2014
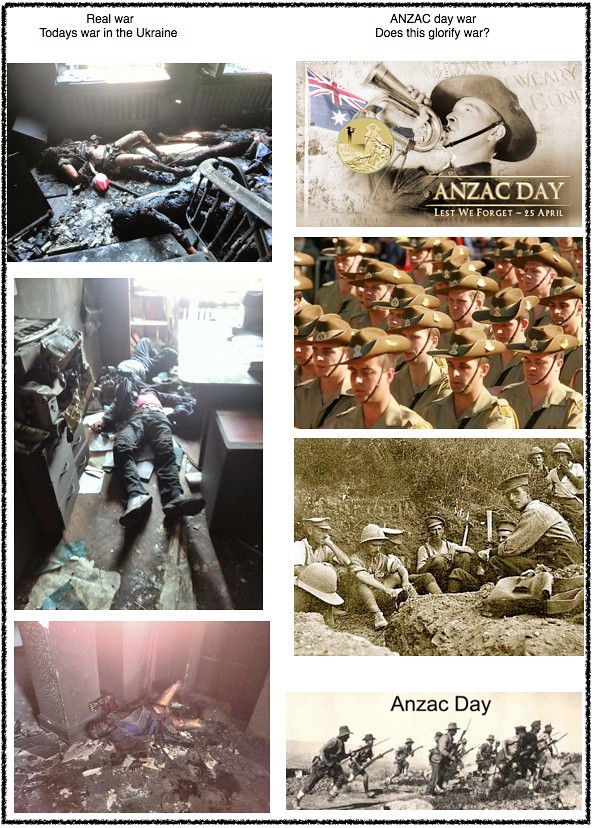
Glorify war
Does ANZAC day glorify war? Possibly. Here are some images of war. On the left is todays war in the Ukraine. On the right is the type of images you see of ANZAC day in Australia. There is nothing wrong with these ANZAC images, in fact it is good to see them. The problem is the images that you don’t see about war and the ANZAC tradition. Compare the images on the right and the left. The wars the ANZACs have fought in would have many of the same images, of what the bad guys have done to us and what we have done to the bad guys. There is concern if we forget that the images on the left are the “main game” images of war and not the images on the right. I think we have forgotten this at least to some degree.
Monday, April 7, 2014
Teenager separation or teenager transformation
“The successful transition of adolescence does not assume the youth detach themselves from their parents. In fact, the transition to autonomy and adulthood is facilitated by secure attachment and emotional connectedness to the parents. This shows that connection (secure attachment) and separation (autonomy) are two sides of the same attachment coin. Attachment security fosters exploration and the development of new competencies thus facilitating the development towards autonomy.
As the youth moves towards autonomy (forming outside the family attachments) it is crucial they have enduring availability and responsivity from the parents as a secure base. At the same time they are moving into a period of identity negotiation and relationship transition with the parents that is inevitably conflictual in nature. Thus the transition from adolescence involves both sustaining connectedness and moving towards individuation, simultaneously.” (Moretti & Holland)
What these people are presenting is an oxymoron. They are saying:
As the parent teenager attachment becomes less important in the teenagers mind
the
parent teenager attachment becomes more important in the teenagers mind.
They are indeed presenting is a tripartite system instead of the usual dual process of separation and individuation.
They are saying there is
Separation
Transformation and
Individuation
Crucial to this stage is:
1. Separation from parents to an identity of autonomy
2. Individuation of self to develop ones own identity
3. Transformation . In order to separate one maintains an attachment to the parents and that relationship with then transforms.
For separation to be complete it must survive the transformation process.
In one sense it could be said that there is not really any separation from the parents only a transformation of the relationship. The separation is just one subset of the overall transformation process. In the transformation process, at least initially, the teenager becomes less separate form the parents. In this sense it could be seen that they are going backwards and becoming less separate rather than more separate from the parents.
This is an interesting idea. It certainly has direct therapeutic implications in the way one presents the idea of separation to the parents and the teenager. The attachment to the parents does not disappear indeed it becomes more important to the teenager!
Consider this diagram
Around 13 years of age the child proceeds on line A. It feels a need to spend less time with the parents and feels freer to move away from them geographically. Behind this is the psychological need to go out into different relationships in the world and form secure attachments with others including non family members.
That process is a psychologically onerous one at least to some degree. The adolescent therefore wants a secure attachment with the parents to help cope with the anxiety of doing this. Hence we have line B which is the desire for a secure attachment. As the teenager begins to break away it actually becomes more dependent on the attachment with the parents. In this sense it could be said that it is going backwards. In its desire to become independent from the parents it becomes more dependent on the parents. But as line B shows this is only temporary. As the teenager becomes more secure in its attachments with people other than the parents these then are used as the basis for feeling secure rather than using the parents for that basic sense of security.
In the graph I have drawn this as occurring between the ages of 13 and 15 years. This of course varies depending on the teenager, the parents and the ability of all parties to handle this process.
Interestingly, I have in the past intuitively referred to this stage as the borderline stage of adolescent development and now with the clarification of these concepts it makes sense of my observation. What I mean by this is the young adolescent begins to behave in a similar fashion as does the borderline personality. In particular the way a teenager relates to his parents has a similar quality to how the borderline personality relates to others in their life.
To quote from the DSM 5 on the borderline.
“The essential feature of the borderline personality is a pervasive pattern of instability of interpersonal relationships, self image and affects, and marked impulsivity...”
“Frantic efforts to avoid real or imagined abandonment.”
“A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation.”
Some of these qualities can be seen in how the young adolescent relates to his parents and indeed his/her first romantic partners. This especially becomes apparent when the parents hold on too tight.
It is not uncommon for parents to bring their teenager to counselling when this is happening. The volatile unstable family relationships are onerous for all concerned and they seek some kind of help to reduce these (borderline like) ways of relating.
Graffiti
Friday, March 14, 2014
Therapy and emergence of the self
Been working with this woman over the past few months and I am doing almost completely relational work. She is pleasant, well versed in therapy, quite capable of introspection and seems motivated. All the qualities are there for a good prognosis.
But it is one of those times where you know something is wrong but you don’t know what it is. You know something is not going right but you can’t articulate it. My Free Child is reacting to her and the therapeutic relationship with disquiet. We have discussed this “problem” I have but it still is not getting to the core of it. My feeling reaction is one of unease. Not in a bad way but in a way of, “I know there is something going on here but I don’t know what it is”.
The work we are doing would be consistent with what Winnicott called the holding environment. I am psychologically ‘holding her”. This of course fits with a relational approach where the focus is on the relationship we have. I have come across the term in relational theory called - the emergence of the self. This fits for what I am doing here. I am simply letting myself go in the relationship with the client not knowing what is going to emerge for me personally.
Winnicott's therapeutic approach of the holding environment does this, but only psychologically. I must say I have always been a bit surprised how people can regress as they do in the holding environment. Indeed some people can become highly regressed. The perfect opportunity for hypnotic suggestions. Getting the client out of the chair down on the floor to do floor work can result in a signficant and abrupt change in ego states especially when they have done it a few times before and are used to it.
I have always thought this a little odd as the therapy in one sense is more about me than about the client. The focus is on my FC and how it is reacting and emerging in relation to the client. Of course the positive for the client is that as I become aware of my personal emergence I report this to her which benefits her. In this instance I don’t feel I have a choice. The conventional approach of analyzing the client, is going OK, but my intuition tells me I am missing something.
What is going to happen? I don’t know. I will have to wait and see what emerges.
Graffiti
Labels:
free child,
holding work,
relational contact,
therapy
Thursday, March 13, 2014
Human development
Developmental psychologists have tended to divide up the human life span into the following three categories. Most books on human psychological development use this breakdown.
One can portray human development as a series of hurdles of tasks that the person must jump over or master. For example in childhood the child has to learn to walk, talk, be toilet trained, deal with the oedipus complex, go to school and so on. They need to go through all the stages of cognitive development and moral development and so on. A child goes through a period of significant and quite fast physical change and psychological change.
One can say the same applies for the teenager. They have a whole series of hurdles to jump or tasks to master. They also have to go through a series of cognitive and moral development stages, learn how to engage with the opposite sex, develop a social support system with their peers and so forth. Like in childhood they go through a period of quite fast and significant physical and psychological development.
Developmental psychologist have decided to make a separation between the stages of childhood and adolescence. This corresponds with the age about when puberty starts. For some reason at this point they say a person has moved onto a new stage of psychological development. They distinguish between the psychological stage of childhood and the psychological stage of adolescence as occurring when puberty arrives.
To my mind this is an arbitrary distinction which is a nonsense and I have not heard of the rational for doing this. One could argue that this distinction needs to be made because the developmental tasks required in childhood are significantly different than the developmental tasks required in adolescence. This is a hypothesis with which I would agree. Without a doubt a 4 year old child is dealing with very different developmental issues than a 14 year old teenager. However the choice of 12 or 13 years of age for the new developmental stage to arrive seems quite a random decision to make.
It can also be argued that a 2 year old child and an 8 year old child are very different physically and the psychological developmental issues they are dealing with are also quite different. So why not conclude that they are two separate developmental stages instead of including them in the same developmental stage as is currently the case. The same of course applies for a 13 year old and the 18 year old. At the moment they are in the same developmental stage but they are also quite different physically and psychologically. Why are they not defined as two separate developmental stages?
One can really see the two stages of childhood and adolescence as one developmental stage. In both stages the young person is going through significant and rapid physical and psychological change. Whereas in adulthood this is not the case. Yes there is indeed physical and psychological change occurring in adulthood but it can be seen as much slower and less psychologically significant. Thus there is much more focus on the younger person as this is where more of the difficulties can occur if the development is not occurring as it should. Developmental psychology is about developmental change in the person so one could see the human life cycle in a different way. Divided up into phases where there is a lot of psychological change occurring and not.
In this model pre-adulthood (childhood and adolesence) is seen as a phase of significant physical and psychological development. Adulthood is a phase of much less significant physical and psychological development. At the end of life we have another developmental stage, Post-adulthood. One could say this stage begins in the late 50s or 60s. In this period there is significant physical change as the body again moves into such a phase of change. These changes can have significant consequences including major disability, deformity or death. These changes force the person into significant psychological change as they accept, or seek to deny, the consequences of such change and acceptance of their bodily changes. With the physical changes the person has to change their perception of them self and their interaction with others and the environment. Thus one could argue that this constitutes a significant level of psychological change and hence we have another period of the development cycle.
For instance the loss of sight, hearing, memory, physical abilities and many other conditions like Parkinson's disease all require the person to make a significant psychological readjustment about how they perceive them self, their identity and how they interact with the world. Of course with illness and accidents these can occur in the adulthood stage and also result in disability and or disfigurement. Again the person has to change their perception of self and the world like happens in the Post-adulthood stage.
This model is about periods of developmental change and periods of non significant change which seems to be the task for the developmental psychologist. In the beginning of life there is a period of significant physical and psychological change. To arbitrarily break this up seems to be a nonsense. This is followed by a period of about 30 to 40 years where there is much more consistency in ones physical and psychological state such that much less psychological development and change occurs. Finally in the last couple of decades of life one again goes into a state of significant physical change. It is postulated that this would then result in significant psychological change as the person reorients their identity and perception of self to correctly align with their physical self.
Graffiti
Labels:
adolescence,
adulthood,
child development,
childhood,
teenager
Saturday, February 15, 2014
Six dilemmas for drug and alcohol therapists
Introduction
When asked to write this article for the UKATA magazine I thought I would do the usual thing and explain a Transactional Analysis theory of addiction that I provide in my book (White(2012)). Instead I decided to do something a little different. The counselling of drug users has some unique difficulties in it, that other forms of counseling do not, such as counselling depression or insomnia.
These are presented here. Six dilemmas the drug counselor will inevitably come across. Six dilemmas that are all to some extent unresolvable but yet the counselor must deal with them when presented by the client.
Dilemma 1. Duality of information on alcohol and drugs in society
A difficulty in treating problematic drug and alcohol use is that drugs are a political issue. Consequently, the circumstances around drug use and particularly about drugs and their effects are confusing. This results in an ongoing duality of information one finds about drugs that are out in the public arena.
In public health discussions one finds, not only in the press, but also stated by public health officials and in health department information which suggests that drugs and alcohol are very dangerous and can result in all kinds of psychological and physical disorders. The impression one tends to get is that drugs are very dangerous and can seduce our young people into serious drug addiction. For example, the youth of westernized society are experiencing an epidemic of amphetamine and crack cocaine at the moment.
However the mainstream literature on drug counselling and finds quotes like, “Contrary to popular belief, most people who use substances do so in ways that cause them relatively little harm. Their use does not interfere significantly in their lives or the lives of others in terms of negative consequences’, (p.13) (Marsh and Dale (2006)). This view would not be held by all substance abuse counsellors but it is fair to say that it is held by many in the field of mainstream substance use counseling.
So we find ourselves in an odd situation where two quite contradictory pieces of information travel along in parallel in society about an important social issue. Both sides openly state it but it is often contradictory.
It seems paramount that any counsellor is well informed about the area in which they are working. This means the person working with substance users must go directly to the scientific literature, journals and books on therapy. They cannot rely on public heath information particularly about the psychological and physical dangers of substance use. Governments are political organizations and drugs are a political issue, hence the negative effects of drug use will tend to be exaggerated so as to fit the current political agenda of the current government. Most governments tend to have some kind of “war on drugs” platform. Public health information on drug use will tend to misrepresent the actual consequences. Sometimes that misrepresentation is small and at other times it is large. However it is essential therapists have accurate Adult information about the area in which they are counselling and hence with substance use one has to go to the scientific literature directly.
Dilemma 2. Scare tactics
This leads directly to the next dilemma for drug counselors. The involves the use of scare tactics by therapists. This is commonly done often without therapists even being aware they are doing it. It involves the exaggeration of the dangers of drugs. The motive behind this is a noble one. “If I can scare the person about the dangers of drugs then they will be less likely to use”.
The counsellor may say to a young drug user, “Marijuana use can lead to schizophrenia”. However sooner or later the young drug user will realize he has not been told the truth, or at least the whole truth. After being told this he will go out and observe his friends smoking and see that not many, in fact very, very few develop a psychosis. The vast majority of marijuana users will not know anyone who develops a psychosis because the numbers where it happens are so small.
He will begin to realize that his therapist has lied to him (by omission) on an important piece of information. What effect will this have on the therapeutic relationship? Not good effects it seems safe to say. At the very least the therapist will loose credibility in the eyes of the client.
However, and this is where we get to the very difficult dilemma for the counsellor, if he tells the client the whole truth then he would say, “Marijuana use can lead to schizophrenia but that will only happen in a very small number of people and if there is no family history of psychosis or pre-psychotic signs in you then it is very unlikely to happen to you.” If the young client hears this what is he possibly going to think. It could be argued that it gives him permission to use marijuana because you have basically told him it’s safe. Of course the counsellor does not want to do that.
Thus we have the dilemma. Don’t tell the whole truth to the client and later he learns he has been lied to and you loose credibility. Do tell the whole truth which gives the client some permission to use. A difficult situation for the therapist indeed.
Dilemma 3. The therapist’s drug and alcohol use
From time to time a client will ask the therapist about their history of alcohol and drug use. It is reasonable to assume that a number of clients would wonder about this as the transference with the drug counsellor increases. I have been asked the question a few times over the years which leaves the therapist in a dilemma. How does one respond to that question? In essence there are two ways to respond. One to answer the question and the other not to answer the question.
Some don’t answer the question because:
1. They are ashamed of their history because they have had a problematic substance use in the past.
2. If they have had some use they may think the client will loose respect for them and they are hypocritical in suggesting the client does not use drugs.
3. If they have had little or no substance use they may think the client will loose confidence in them because they don’t know what they are talking about.
4. They see it as a private matter and simply not wish to disclose that to the client.
If one refuses to answer the question because they say it’s private or by using a tangential response like, “Why is that important to you?”, it seems reasonable to assume that the client will still wonder why the therapist refused to answer the question. They will then consider the options listed as the real reason. It builds unwanted conjecture and intrigue in the mind of the client. Having said that it is by no means a significant rupture in the therapeutic relationship.
If one answers the question reasonably honestly and is believed by the client then they are not left with any unwanted intrigue but the client may then think the first three options listed above. This of course is also not conducive to the smooth functioning of the therapeutic relationship. Another dilemma for the therapist of substance users.
Dilemma 4. The harm reduction contract
The next dilemma relates to the harm reduction contract. Harm minimization is widely practiced in the addictions field. It involves working with the client such they become informed about the potential dangers of drug consumption. For instance injecting drug use is more dangerous oral drug use. Or using drugs when there is a possibility of overdose such as with heroin, using alone is more dangerous than using when others are there such that they can help if an overdose occurs.
A significant problem with this aspect of counselling is that many drug users know the dangers but do not alter their behaviour because of that knowledge. This has lead to the concept of negotiated safety. The therapist and drug user negotiate what safety strategies they are prepared to use. In essence the therapist is asking the client to make a contract about what they are willing to do in their drug taking. To assist with this is the idea of a harm reduction contract (HRC). The client makes a contract about the behaviour they will use and for how long the contract lasts.
The HRC involves the client making a short statement to self (in the presence of the therapist).
“I contract with myself to stop (the potentially harmful behaviour) and to (the harm reduction behaviour) for ‘x’ amount of time.”
For example:
“I contract with myself to stop sharing injecting equipment and to use only my own equipment for four days”.
“I contract with myself to stop using heroin alone and only use when there are others around me for two months”.
Whilst such HRCs can be useful in increasing a drug users safety it can also cause problems, in two possible ways. First it can have a negative result on the therapeutic alliance. Consider these two diagrams presented in White (2012)
Diagram 1. Harm reduction contract using the Adult ego state.
Diagram 2. Harm reduction promise using the Child ego state.
White (2012) (p.105)
This applies to any therapeutic contracting but particularly to the HRC (and the no suicide contract (NSC)). Any contract must not become a promise in the mind of the client. If it does then it is highly likely the contract will not last successfully. Of course it is most important that a HRC and NSC do work. If they do not the potential outcomes are more significant than other contracts about non life threatening matters.
In the transference relationship there is pressure on the client to begin seeing the therapist as a parent figure. The more this occurs the easier it is for a contract to change into a promise in the eyes of the client. In the transference they tend to become more childlike around the therapist and that will include childlike in their contracting such that contracts may start to become promises instead. As I stated this is unwanted for the long term outcome of the contract.
However if this promise making process occurs over time, as it can indeed do, that can create quite a significant rupture in the therapeutic alliance. In working with the therapist the client knows at some level that they are not contacting and instead are making a promise to the therapist. Of course this can remain a secret which the therapist does not know about and thus can undermine the therapeutic alliance.
If one does not do such contracting the likelihood of a therapeutic rupture diminishes but then one cannot make a HRC and the client is put at higher risk. Hence we have the dilemma. There are other objections to contracts such as the HRC and NSC, which in particular come from family therapy. This approach sees such contracting as supporting and encouraging the idea of the ‘Identified Patient’, which of course is a negative in family therapy theory.
In my experience problematic drug use can sometimes be due to a dysfunctional family structure. This is not always so, but can be the case to varying degrees with some clients, particularly younger clients. Henceforth if one uses the HRC that is supporting the dysfunctional family system. On the other hand if one does not use the HRC the client is left at higher risk. A further significant dilemma for the therapist that can have potentially fatal outcomes.
Dilemma 5. Closing escape hatches
Following on from the previous point, when working with dependent drug users one not uncommonly comes across clients with varying degrees of suicidality. When this happens one is left with the dilemma of closing the suicide escape hatch or not.
The choice of the word “escape hatch”, originally by Holloway (1973), was an apt one. Most people would consider an escape hatch a comforting thing to have. Most people like to have a Plan B, if Plan A does not work out satisfactorily. The suicide escape hatch could be see as a Plan B type of situation that would make people feel more secure.
Also, White (2011) notes that having a suicide escape hatch can provide a method of self soothing expressed in a masochistic form. Closing the escape hatch may remove one of the individual’s important methods of self soothing. Consider the following client report:
“Having the option there in the back of my head actually serves to help me. It doesn't help once the danger is more immediate. When it starts making messes. But on a day to day basis it is nice....I visualize the method in my head a lot though during times of stress. It's soothing.” (White (2011)(p.240))
Another client, who had previously made two serious suicide attempts reported that he gets images in his mind up to ten times per day. It is the image of him hanging himself in a tree. He reports that he does not think of conjuring them up instead they tend to spontaneously arise in this consciousness. When he has the image he feels reassured and a sense of calmness. He has in essence developed a ritualized suicide fantasy about how he would try to suicide if the circumstances arose. This masochistic ritualized fantasy or escape hatch provides a way for him to self soothe.
To close the escape hatch is to remove the fantasy, or Plan B, which for some as we can see above means to remove a method of dealing with stress. If that happens they will be in worse condition and hence be at a higher risk of a suicide attempt. However if the client does not close the escape hatch they are still leaving suicide open as an option for them. Thus we are left with the dilemma.
It should be noted that this only applies to some suicidal people. Others when offered the option of closing the suicide escape hatch can experience relief. It’s as though the therapist is giving them permission to live when he suggests closing the escape hatch. Obviously the same dilemma is not apparent with these individuals.
Dilemma 6. Pharmacotherapy
A widely used way to treat drug dependence is with pharmacotherapy. One treats the drug abuse by using medications in various ways. Common examples are treating opioid dependence with drugs like methadone, buprenorphine and naltrexone. Or alcohol addition can be treated by using antabuse. Around the world today these are widely practiced.
Pharmacotherapy for treating drug addiction has an inherent contradiction in it. It says to the client - “Take this drug to stop taking drugs”. A double message is being given to the client. In substance use counselling, the therapist by their very presence in the counseling session, is saying to the client, “It is a good idea not to use drugs or to reduce your drug use.” The very act of working with a drug using client communicates this to the client. You are engaged in therapy with them and that is obviously not about encouraging their drug use. The therapist is seeking to discourage in some form the client’s drug use. That is why the therapist is there in the first place.
On the other hand if the therapist is providing drugs for the pharmacotherapy treatment or is supportive of the pharmacotherapy it can be argued gives permission to the client to take drugs. The very act by the therapist of engaging in pharmacotherapy with the client says to the Child ego state of the client, “It’s OK to take drugs”. Of course we can provide all the Adult ego state explanations of why taking methadone is different to taking heroin and they are all true. There are clear differences. At the same time the very act of giving a client a drug to take, no matter what it is, gives permission to the Child ego state to take drugs.
Unfortunately as far as the Child ego state is concerned actions speak louder, often much louder than words. This is not meant to be an argument against the use of pharmacotherapy for the treatment of drug addiction. I have seen methadone be very useful for some opiate users. What is being highlighted is the dilemma and that we must be clear about what we are communicating to our clients. With pharmacotherapy we are giving a double message and of course one does not want to do that. At the same time pharmacotherapy can be a of considerable assistance in treating drug addiction. A dilemma indeed.
Conclusion
The article set out to identify some of the dilemmas a drug counsellor has to deal with. There are more but word limitations prevent those from being articulated. However it is safe to say that six of the most common are described here.
As mentioned before these do not have obvious answers and thus need to be dealt with on a case by case basis. The solution in each situation depends on the clinical features of the client and the type of therapy being used at the time. The solution varies from situation to situation depending, as I said, on the clinical circumstances apparent at the time the dilemma surfaces.
References
Holloway, W.H. (1973). Shut the escape hatch: Monograph IV. The Monograph Series. Ohio: Midwest Institute for Human Understanding.
Marsh, A. and Dale, A. (2006) Addiction Counselling. Melbourne: IP Communications
White, T. (2011) Working With Suicidal Individuals: A Guide to Providing Understanding, Assessment and Support. London: Jessica Kingsley Publishers.
White, T. (2012) Working with Drug and Alcohol Users. London: Jessica Kingsley Publishers.
Labels:
addiction,
alcohol,
drugs,
escape hatch,
no harm contract,
pharmacotherapy
Thursday, February 13, 2014
Monday, January 13, 2014
Saturday, January 11, 2014
Some therapeutic observations of the AA approach
Having worked with many who have embraced the AA approach as a way to stay clean and sober I find I am left with some favorable comments to make about it.
Regardless of whether one agrees or not with the ideas of a higher power being responsible for one’s alcoholism or substance use I intend to just look at the some aspects of the AA approach irrespective of the underlying philosophy.
At the moment I am working with a number of people who are in the maintenance stage (of the stages of change model). They have been clean and sober for a number of years ranging from 2 to 10 years. With all of them the possibility of their relapse arises from time to time and represents a fear to them in varying degrees.
In my view the way they have learnt to use the AA approach which makes it particularly suitable to the individual who is in the maintenance stage.
1. The self regulating aspect of the AA approach. As it is free and available everyday of the year one can regulate their own attendance at meetings. It can range from once every few months to a number of times daily. When their maintenance is a bit shaky commonly they will increase their rate of attendance at meetings.
In most counselling situations this can not occur. It may get too expensive and most often the person has to make appointments with the counsellor such that they have to wait days if not weeks to meet. Even if it is free or they can afford it most counsellors don't really see the same client a number of times a day or every second day and so forth. In most counselling situations the ability for the person to self regulate contact is not permitted in the same way it is with AA.
2. The sponsor system. In my view another helpful aspect of AA that is used well by some of those at the maintenance stage to assist with their sobriety. The fact that they aren't trained counsellors and bound by lists of codes of conduct actually has a positive result in one way. It allows for a truly mentor type of relationship that one can only get with that type of informality.
The formal therapeutic relationship between client and therapist actually creates quite a rigid structure in the relationship. In addition AA sponsors tend to have much more flexibility in their availability of contact. One of the reasons being that they have far less people ('clients') to be available to. This again allows for a person to self regulate their contact with the sponsor as they feel the need (at least to some degree). In the usual therapy relationship this self regulation by the client is far less flexible, again highlighting the rigidity one finds more in the usual therapeutic relationship.
The 12 step programme. At times those seeking to maintain sobriety can put themselves back onto the 12 step programme (self regulation again). With their sponsor they start again at step one and go through the programme. This seems to provide some with a more secure base. It gives them something to focus on and do that they see as protecting self. Also it is not a short programme taking, not days or weeks, but months. The individual places self on a long process which they see as part of their arsenal to fight addiction thus feeling protected in this sense. And as I said before it gives them something to focus on and do instead of using alcohol or drugs.
Overall I have found some at least use the AA (or NA) approach in these ways which certainly helps them to remain clean and sober.
The other thing which must be noted is that AA is not therapy and is not attempting to be therapy. At least in the sense of helping people to resolve their childhood traumas, make redecisions, deconfuse and decontaminate and so forth. This raises an interesting issue. Is it possible to take some of these positive aspects of AA and weave them into a form of mentor relating? I purposely don’t use the word therapy because as soon as you do that you immediately impose all sorts of conditions and implications on the process and hence you loose the flexibility and as I said end up with quite a rigid relationship style.
Is it possible to find an in between ‘spot’. You are not therapist and client but you have two people relating who happen to be a therapist (which I will refer to as a mentor) and a clean drug user. The relationship would allow much more flexibility in how the ex user can contact the mentor and the mentor does not have to respond in a therapeutic manner. Instead one could develop some kind of ‘step’ programme like AA has and the ex user and mentor could do that as well of course the relationship things which would firm up the person’s resolve not to use. Of course this could only be done with a very few ex users as the mentor would become over loaded. Also of course ti would not have to be kept to just drug and alcohol use problems.
Graffiti
Labels:
12 step programme,
AA,
alcohol addiction,
drug addiction,
Therapists
Subscribe to:
Comments (Atom)